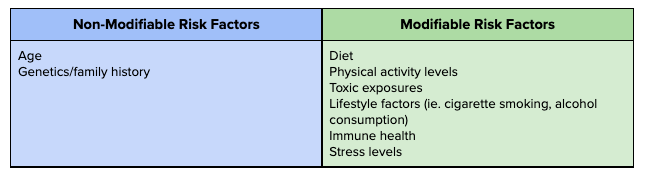
It is easy to overlook the importance of dietary choices in safeguarding against various ailments. One such silent protector in our diet is fibre, a nutrient with profound implications for our digestive health and, notably, in the prevention of colorectal cancer. Colorectal cancer is the 4th most diagnosed cancer in Canada[i], and lifestyle factors such as diet can play a significant role in its development.
At Saskatoon Naturopathic Medicine, we practice a comprehensive approach to wellness, and understanding the role of fibre in colorectal cancer is paramount.
What is fibre?
Fibre is the portion from plant-based foods that our bodies cannot fully digest and end up being fermented or broken down by the bacteria that live in our digestive tracts (called the gut microbiome).
The fermentation of fibre by our gut bacteria produces short-chain fatty acids (SCFAs) including butyrate, which is the main source of energy for colon cells.
Why is fibre important?
Fibre helps move substances through our GI system, thereby facilitating the elimination of carcinogenic substances. Additionally, the SCFAs (including butyrate) have anti-inflammatory, immune-modulating, and anti-carcinogenic effects on the cells of our colon and help slow the growth of colon cancer cells.
Gut Dysbiosis
Our diet plays an important role in balancing the bacterial populations that make up our gut microbiome. Diets that are higher in fibre help to promote bacteria that produce butyrate and reduce inflammation. Diets low in fibre can lead to gut dysbiosis (a decrease in the beneficial bacteria and an increase in bacteria that promote inflammation).
We believe in empowering our patients with actionable steps to optimize their health. Here are some practical tips for incorporating more fibre into your diet:
Embrace whole foods over refined, highly-processed options.
Load up on produce, aiming for a colorful variety to maximize your nutrient intake.
Snack smart to curb cravings and boost fibre intake throughout the day.
Experiment with legumes in soups, salads, and stews.
Great sources of fibre for fermentation, butyrate production, and promoting microbiome diversity include soluble fibres such as:
Beta-glucans – oats, barley, sorghum, rye, mushrooms
Pectins – Apples, oranges, apricots, white beans, black beans
Inulin – Agave, artichokes, asparagus, bananas, chicory root, garlic, onions, leeks, wheat
A diet rich in a variety of dietary sources of fibre is beneficial for health – it helps substances move through the gut, balances sugar and cholesterol levels, and promotes a healthy gut microbiome. Aim for 30 grams of fibre per day from foods including grains, vegetables, fruits, legumes, nuts and seeds.
We stand committed to guiding you on your journey to vibrant health, one fibre-filled meal at a time.
[i] https://www.colorectalcancercanada.com/colorectal-cancer/statistics/
Sources:
Fratila, T. D., Ismaiel, A., & Dumitrascu, D. L. (2023). Microbiome modulation in the prevention and management of colorectal cancer: A systematic review of clinical interventions. Medicine and Pharmacy Reports, 96(2), 131–145. https://doi.org/10.15386/mpr-2526
Madrigal-Matute, J., & Bañón-Escandell, S. (2023). Colorectal Cancer and Microbiota Modulation for Clinical Use. A Systematic Review. Nutrition and Cancer, 75(1), 123–139. https://doi.org/10.1080/01635581.2022.2108468
Rinninella, E., Mele, M. C., Cintoni, M., Raoul, P., Ianiro, G., Salerno, L., Pozzo, C., Bria, E., Muscaritoli, M., Molfino, A., & Gasbarrini, A. (2020). The Facts about Food after Cancer Diagnosis: A Systematic Review of Prospective Cohort Studies. Nutrients, 12(8), 2345. https://doi.org/10.3390/nu12082345
Holscher, H. D. (2017). Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes, 8(2), 172–184. https://doi.org/10.1080/19490976.2017.1290756
Bashir, K. M. I., & Choi, J.-S. (2017). Clinical and Physiological Perspectives of β-Glucans: The Past, Present, and Future. International Journal of Molecular Sciences, 18(9), 1906. https://doi.org/10.3390/ijms18091906
Ross, J. K., English, C., & Perlmutter, C. A. (1985). Dietary fiber constituents of selected fruits and vegetables. Journal of the American Dietetic Association, 85(9), 1111–1116.
Tosif, M. M., Najda, A., Bains, A., Kaushik, R., Dhull, S. B., Chawla, P., & Walasek-Janusz, M. (2021). A Comprehensive Review on Plant-Derived Mucilage: Characterization, Functional Properties, Applications, and Its Utilization for Nanocarrier Fabrication. Polymers, 13(7), 1066. https://doi.org/10.3390/polym13071066
Dhingra, D., Michael, M., Rajput, H., & Patil, R. T. (2012). Dietary fibre in foods: A review. Journal of Food Science and Technology, 49(3), 255–266. https://doi.org/10.1007/s13197-011-0365-5