First off, what is cholesterol anyway?
Cholesterol is a waxy, fat-like substance that is produced by your liver. Cholesterol is actually vital for many different structures and functions in the body such as the formation of cell membranes, hormone production, and the synthesis of vitamin D from the sun. So if it plays all of these key roles, why are we so concerned when cholesterol levels get high?
You may have heard by now that we have “good” (HDL) and “bad” (LDL) types of cholesterol. HDL and LDL stand for high density and low density lipoprotein. These are particles made from fat and protein that attach themselves to cholesterol to transport them throughout the blood stream. LDL is associated with the bad form of cholesterol as its function is to carry cholesterol to the arteries. When LDL levels get too high it may collect in vessel walls and contribute to plaque formation (atherosclerosis) in addition to increasing your risk of heart disease and stroke. HDL on the other hand functions by transporting cholesterol back to the liver – almost like a clean up crew- to prevent blood cholesterol levels from getting too high. So when cholesterol gets returned to the liver – what happens next? In the liver, cholesterol is secreted directly into bile where it is then secreted into the intestines. This is where optimizing gut health comes into play.
Once cholesterol reaches the intestines one of two things can happen. One, the bile is removed from the body via fecal excretion or two, the cholesterol is re-absorbed by enterocytes (cells that line our gut) and returned back to circulation. The intestine typically absorbs about 50% of the cholesterol presented to it – but this can vary from 20%-80% depending on the person. Of the absorbed cholesterol, approximately 80% comes from bile and only ~20% comes from diet (which is why eggs might not be so bad after all). Given that it seems our bodies own production and subsequent elimination of cholesterol seems to be the larger issue, how can we help swing our reabsorption percent from 50-80% down to 20%?
FIBER:
Soluble fiber can reduce the absorption of cholesterol into your blood stream. Insoluble fiber decreases intestinal transit time thus promoting regular bowel movements to ensure your LDL cholesterol is being eliminated efficiently. It is suggested to consume between 25-30g of fiber per day.
Soluble fiber foods: Brussels sprouts, avocados, flax seeds, and black beans
Insoluble fiber foods: nuts, beans and vegetables, such as cauliflower, green beans and potatoes
Probiotics:
Probiotics are healthy bacteria found in our gut. Fermented foods contain them and fiber containing foods feed them. Probiotics are suggested to reduce cholesterol by deconjugating bile acids, using cholesterol for nourishment, and/or incorporating cholesterol into the cell wall of the probiotic bacteria. Probiotics also help to keep us regular which decreases the chance for cholesterol to become re-absorbed.
Sources of probiotics: yogurt, sauerkraut, kimchi, kombucha, miso, tempeh, pickles.
Lastly, outside of gut health and moving more into diet in general, the Mediterranean diet has been shown to be an effective approach to supporting healthy cholesterol levels. The Mediterranean diet includes the following:
Increased Omega 3 consumption:
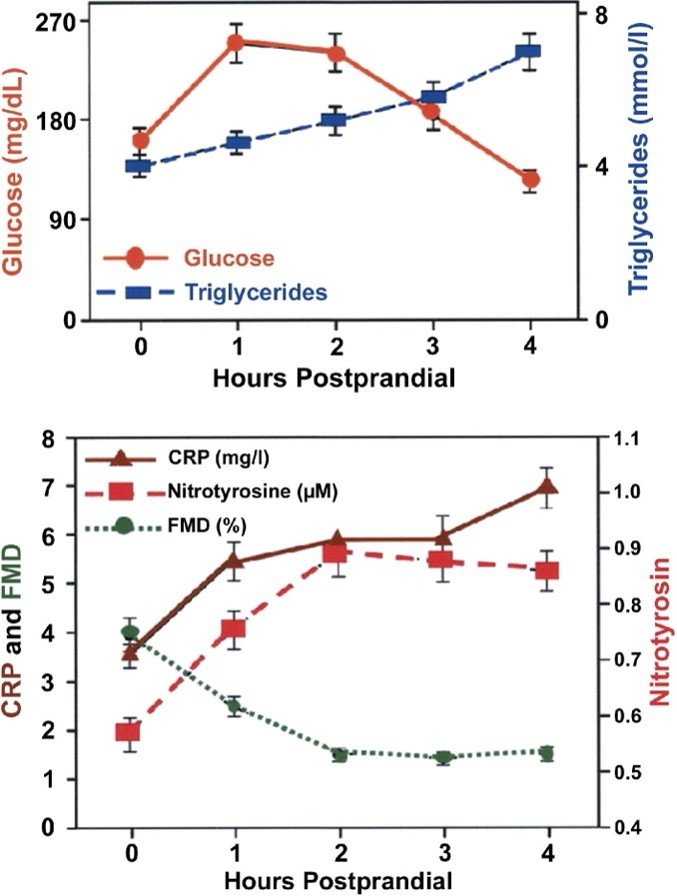
Foods high in omega 3’s can increase HDL while reducing triglycerides — a type of fat found in blood — as well as reduce your blood pressure and risk of developing blood clots.
Omega 3 rich foods: Fish and other seafood (especially cold-water fatty fish, such as salmon, mackerel, tuna, herring, and sardines) Nuts and seeds (such as flaxseed, chia seeds, and walnuts)
Increased consumption of Nuts/Seeds:
Almonds and other tree nuts can improve blood cholesterol levels by reducing LDL. Almonds have been suggested to reduce LDL levels by reducing LDL reabsorption in the gut, increasing cholesterol and bile secretion into the gut, and regulating enzymes involved in cholesterol syntheses.
Olive oil:
Foods that contain monounsaturated fats (including olive oil) may raise HDL (good) cholesterol. The least processed form of olive oil to use is cold pressed extra virgin olive oil.
In health,
Dr. Brittany Pearce, ND., RHN.
References:
Vrins CL. From blood to gut: direct secretion of cholesterol via transintestinal cholesterol efflux. World J Gastroenterol. 2010;16(47):5953-5957. doi:10.3748/wjg.v16.i47.5953
Jesch ED, Carr TP. Food Ingredients That Inhibit Cholesterol Absorption. Prev Nutr Food Sci. 2017;22(2):67-80. doi:10.3746/pnf.2017.22.2.67
Freeman AM, Morris PB, Aspry K, Gordon NF, Barnard ND, Esselstyn CB, Ros E, Devries S, O'Keefe J, Miller M, Ornish D, Williams KA, Batts T, Ostfeld RJ, Litwin S, Aggarwal M, Werner A, Allen K, White B, Kris-Etherton P. A Clinician's Guide for Trending Cardiovascular Nutrition Controversies: Part II. J Am Coll Cardiol. 2018 Jul 31;72(5):553-568. doi: 10.1016/j.jacc.2018.05.030. PMID: 30049315.
Cohen DE. Balancing cholesterol synthesis and absorption in the gastrointestinal tract. J Clin Lipidol. 2008;2(2):S1-S3. doi:10.1016/j.jacl.2008.01.004
Cartolano FC, Dias GD, Miyamoto S, Damasceno NRT. Omega-3 Fatty Acids Improve Functionality of High-Density Lipoprotein in Individuals With High Cardiovascular Risk: A Randomized, Parallel, Controlled and Double-Blind Clinical Trial. Front Nutr. 2022 Feb 23;8:767535. doi: 10.3389/fnut.2021.767535. PMID: 35281761; PMCID: PMC8905646.
Berryman CE, Preston AG, Karmally W, Deckelbaum RJ, Kris-Etherton PM. Effects of almond consumption on the reduction of LDL-cholesterol: a discussion of potential mechanisms and future research directions. Nutr Rev. 2011 Apr;69(4):171-85. doi: 10.1111/j.1753-4887.2011.00383.x. PMID: 21457263.