We all know it’s not ideal to have a diet high in sugar. Most of us know this with respect to managing our weight – but what about the immune system? What about colds, flus, autoimmune conditions, diabetes, cancer – does sugar consumption make us more susceptible? And if it does, how much does it take to make a difference? Before we dive in, lets do a quick review of the immune system.
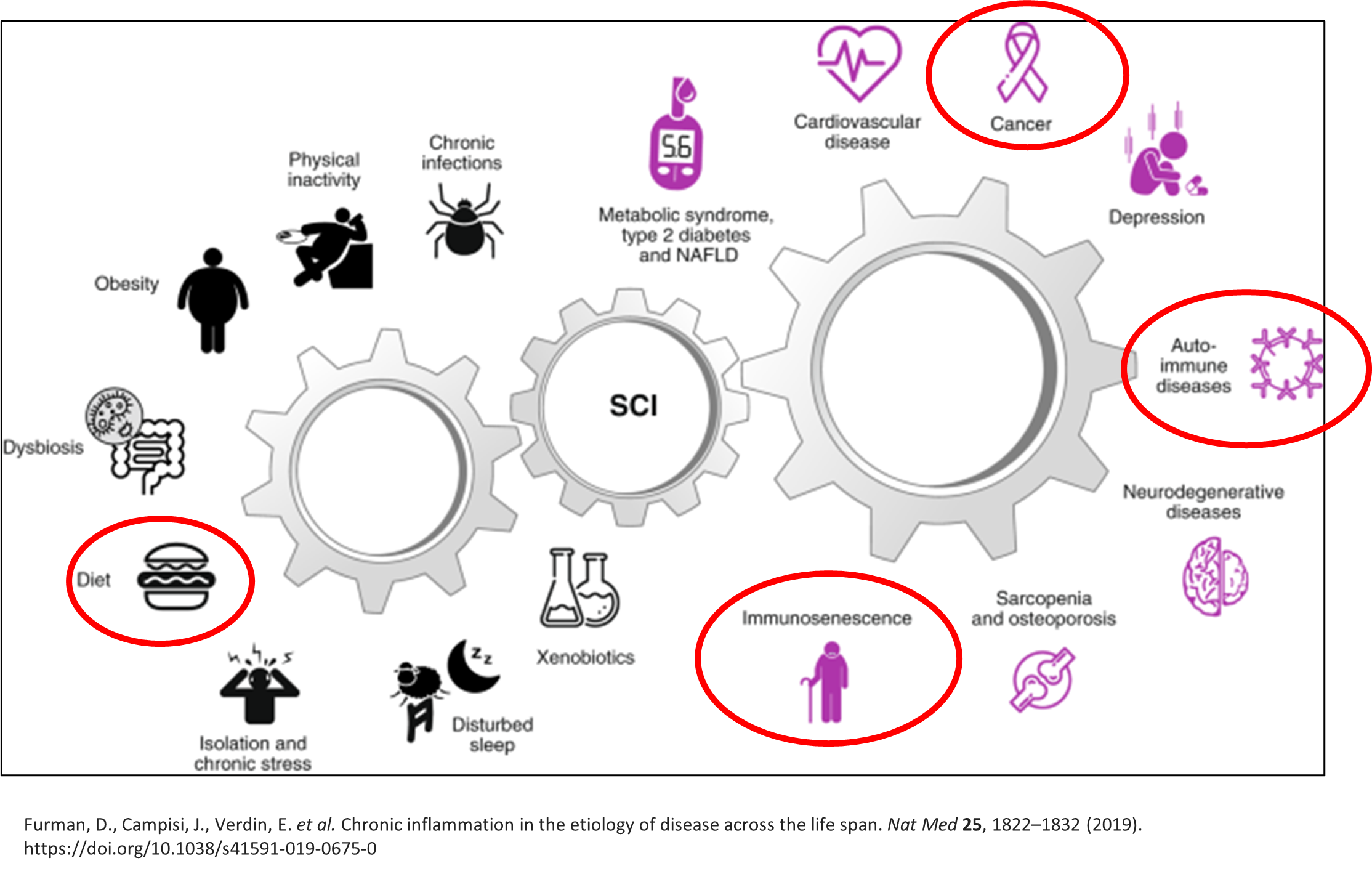
Above you’ll notice two main subdivisions of our immune system. We have our innate immunity, which can be thought of as the offense players and the adaptive immunity which could be considered the defence players. The innate immune system is first to respond (within minutes to hours) when there is a foreign invader. It’s the part of our immune system responsible for mounting a fever and initiating inflammation. Inflammation is useful in the short term for acute injuries or illnesses. Long term however, inflammation plays a strong role in the development of several diseases such as autoimmune diseases, cardiovascular disease, diabetes mellitus, chronic kidney disease, non-alcoholic fatty liver disease and neurodegenerative disorders3. The innate immune response has no memory which means it responds the same way to all encountered pathogens. The adaptive immune system, also known as “acquired immunity” takes days to weeks to kick in. It is very specific and diverse to each type of pathogen it encounters which means it mounts a unique response to each pathogen after it has been “primed” or exposed to that pathogen. The adaptive immune system does have a memory which means it will respond faster the next time you are exposed to that pathogen.
How does sugar affect the immune system?
When we consume foods high in simple sugars, we get a post prandial (post meal) spike in the amount of sugar and triglycerides in our blood[1]. This is also known as “post prandial dysmetabolism” and it induces a wide variety of negative changes in the body. Just one high sugar meal can trigger transient effects such as:
Inhibition of neutrophils[2]
o Neutrophils are part of the innate (first response) immune system. They patrol for foreign invaders and then trap and kill pathogens when discovered. High blood sugar prevents neutrophils from being able to get to the site of microbial infection (inhibition of migration), decreases their ability to trap pathogens (phagocytosis), and furthermore inhibits their ability to kill microbes2.
Increased inflammation and inflammatory markers such as C-reactive protein1
o Long term inflammation (such as with repeated exposure to a diet high in sugar) can cause a breakdown of immune tolerance which may lead to major alterations in all tissues and organs, as well as normal cellular physiology, which can increase the risk for various non-communicable diseases in both young and older individuals[3]. It can also impair normal immune function leading to increased susceptibility to infections and tumors as well as poor response to vaccines3.
Immediate oxidant stress (free radical production)1
o Oxidant stress acutely triggers inflammation which negatively impacts the immune system3. In addition, this oxidant stress also increases LDL oxidation, vessel constriction and clot formation, all of which contribute to cardiovascular disease1.
Endothelial (blood vessel) dysfunction1 2
o High blood sugar decreases blood vessel dilation (reducing blood flow) while simultaneously increasing leakiness of the blood vessels and how quickly the blood clots due to the inflammatory response. This reaction is similar to how a viral infection would trigger vascular inflammation leading to endothelial dysfunction, coagulation and cardiovascular disease[4]. Long term vessel “hyperpermeability” has been associated with increased aging and diseases such as Parkinson’s and Alzheimer’s[5].
Glycosylation of proteins and alteration of tertiary structures of complement2
o While this might sound complicated, what is important to understand is that these changes make it difficult for the body to recognize foreign pathogens and eliminate them2. Changes in glycosylation may increase the inflammatory response, enable viral immune evasion (ability to escape), and promote cancer cell metastasis[6]. Auto-immune disease development such as lupus and irritable bowel disease involve glycosylation of one or more glycoproteins6.
This diagram shows a summary of how systemic chronic inflammation (SCI) develops and what it can lead to.
How much sugar does it take?
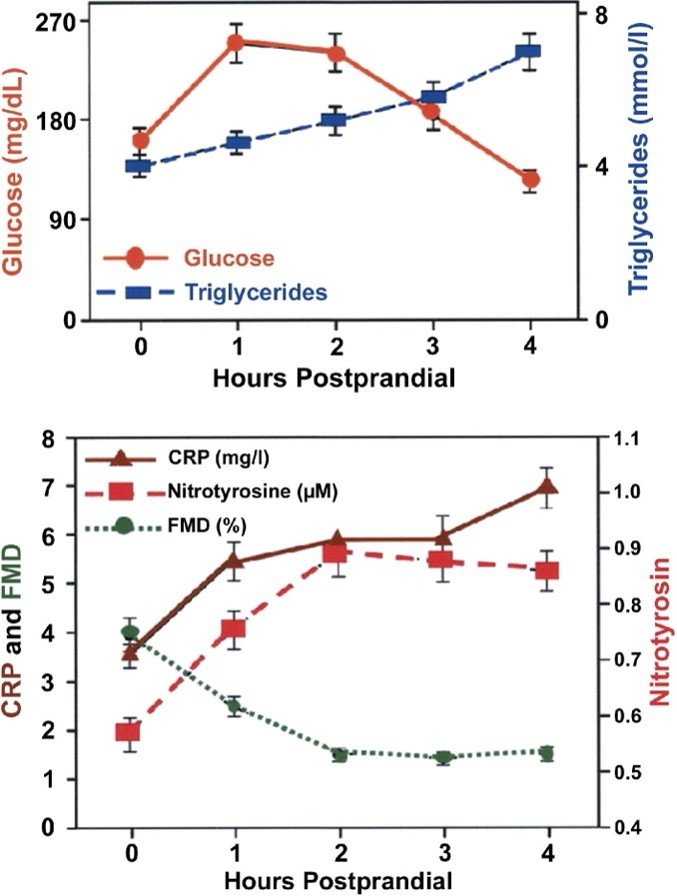
To provide a little bit of context, the chart below shows the immediate effects of consuming a beverage containing 75g of glucose. This amount of sugar is similar to a cup and a half of white rice (68g). You will notice that within a few hours the amount of glucose and triglycerides increase significantly which leads to immediate oxidant stress (nitrotyrosine), inflammation (C reactive protein [CRP]) and endothelial dysfunction via decreased blood flow via reduction in the diameter of blood vessels (FMD).
Another study looking at the immediate effects of sugar consumption found that people who consumed 40 grams of added sugar from just one 375ml can of soda experienced an increase in inflammatory markers, insulin resistance and LDL cholesterol[7].
In addition to the above, high sugar containing meals can alter our gut barrier function and drive gut bacteria imbalances (also known as dysbiosis). This can lead to what is referred to as “leaky gut” or intestinal permeability which fuels inflammation and taxes the immune system further[8]. In addition, altered gut bacteria has been suggested to contribute to a multitude of immune-mediated disorders such as irritable bowel disease [9]. Furthermore, as mentioned above, diets high in sugar have been implicated in the development of all kinds of diseases such as cardiovascular disease, type two diabetes, obesity, non alcoholic fatty liver disease, gout and autoimmune conditions such as rheumatoid arthritis[10].
How much sugar should we have and how can we reduce the negative impacts of sugar on our immune system and overall health?
The Heart and Stroke Foundation recommends that you consume no more than 10% of your total calories per day from added sugar – ideally less than 5%[11]. This means for someone with a 2000 calorie/day diet you should consume less than 48g (10%) of sugar. This is slightly more than one can of pop. The following are some key things you can consider doing to reduce the impact of high sugar foods on your immune system and overall health:
Fiber and low glycemic carbohydrates:
o When eating carbohydrates, try to choose high fiber, low glycemic index (glycemic index <55) foods such as whole grains, beans and legumes, vegetables and berries. Carbohydrates in these forms are much harder to digest thus slowing the rate sugar enters the blood stream.
Protein and fat
o Ensure you consume a healthy source of protein and/or fat with each meal or snack. The addition of protein and fat also helps to slow the rate sugar is released into the blood stream which prevents a spike in blood sugar. An example might be having almond butter with your banana.
o Below on the left is an example of how adding whey protein to the same glucose drink reduced the increase of blood sugar after drinking1. On the right we have an example of how adding 90g of almonds to a high glycemic index meal reduced the area under the curve for glucose by 58%1.
Vinegar:
o Research suggests that 1-2 tablespoons of vinegar added to a meal can lower post prandial glucose by 25%-35% as well as increase post meal satiety by more than two-fold1.
Avoid low glycemic and highly processed foods/beverages
o Avoid highly processed foods and beverages which often contain high amounts of simple sugars, high fructose corn syrup and white flour.
Walk/Exercise
o Walk for 10-30 minutes after each meal[12]. Short walks after each meal were found to be more effective for blood sugar control than one-time daily exercise regimes or the use of metformin alone[13] [14].
Reading food labels can help you make an informed decision on the foods you are eating. Remember, the daily recommended amount of sugar is less than 48g.
Ex: Tropicana – One serving of Tropicana juice is 34g of sugar. This is 72% of the recommended daily intake of sugar. In addition, orange juice in general is considered to have a glycemic index of 66-76 which is considered moderately to very high in regard to how much it will raise our blood sugar.
Another example is BBQ sauce. Bulls Eye BBQ sauce has 12g of sugar/2tbsp. This means that just two tablespoons equal to 25% of the daily recommended sugar intake. However often in meals with BBQ sauce (such as a burger) we are having a bun, and ketchup and french-fries as well. This one meal quickly throws us far over the daily recommended intake.
Working with a healthcare provider can help you pinpoint which risk factors you have and how to safely reduce your risk and support better overall immune health. Be sure to talk with your health care provider before making any drastic lifestyle or dietary changes.
In health,
Dr. Brittany Pearce, RHN., ND.
[1] O'Keefe JH, Gheewala NM, O'Keefe JO. Dietary strategies for improving post-prandial glucose, lipids, inflammation, and cardiovascular health. J Am Coll Cardiol. 2008 Jan 22;51(3):249-55. doi: 10.1016/j.jacc.2007.10.016. PMID: 18206731.
[2] Jafar N, Edriss H, Nugent K. The Effect of Short-Term Hyperglycemia on the Innate Immune System. Am J Med Sci. 2016 Feb;351(2):201-11. doi: 10.1016/j.amjms.2015.11.011. PMID: 26897277.
[3] Furman, D., Campisi, J., Verdin, E. et al. Chronic inflammation in the etiology of disease across the life span. Nat Med 25, 1822–1832 (2019). https://doi.org/10.1038/s41591-019-0675-0
[4] Xu S, Jin T, Weng J. Endothelial Cells as a Key Cell Type for Innate Immunity: A Focused Review on RIG-I Signaling Pathway. Front Immunol. 2022 Jul 5;13:951614. doi: 10.3389/fimmu.2022.951614. PMID: 35865527; PMCID: PMC9294349.
[5] Oakley R, Tharakan B. Vascular hyperpermeability and aging. Aging Dis. 2014;5(2):114-125. Published 2014 Apr 1. doi:10.14336/AD.2014.0500114
[6] Reily C, Stewart TJ, Renfrow MB, Novak J. Glycosylation in health and disease. Nat Rev Nephrol. 2019 Jun;15(6):346-366. doi: 10.1038/s41581-019-0129-4. PMID: 30858582; PMCID: PMC6590709.
[7] Aeberli I, Gerber PA, Hochuli M, Kohler S, Haile SR, Gouni-Berthold I, Berthold HK, Spinas GA, Berneis K. Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: a randomized controlled trial. Am J Clin Nutr. 2011 Aug;94(2):479-85. doi: 10.3945/ajcn.111.013540. Epub 2011 Jun 15. PMID: 21677052.
[8] Camilleri M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut. 2019 Aug;68(8):1516-1526. doi: 10.1136/gutjnl-2019-318427. Epub 2019 May 10. PMID: 31076401; PMCID: PMC6790068.
[9] Zheng, D., Liwinski, T. & Elinav, E. Interaction between microbiota and immunity in health and disease. Cell Res 30, 492–506 (2020). https://doi.org/10.1038/s41422-020-0332-7
[10] Moling O, Gandini L. Sugar and the Mosaic of Autoimmunity. Am J Case Rep. 2019;20:1364-1368. Published 2019 Sep 15. doi:10.12659/AJCR.915703
[11] https://www.heartandstroke.ca/healthy-living/healthy-eating/reduce-sugar
[12] Bellini A, Nicolò A, Bazzucchi I, Sacchetti M. The Effects of Postprandial Walking on the Glucose Response after Meals with Different Characteristics. Nutrients. 2022;14(5):1080. Published 2022 Mar 4. doi:10.3390/nu14051080
[13] Pahra D, Sharma N, Ghai S, Hajela A, Bhansali S, Bhansali A. Impact of post-meal and one-time daily exercise in patient with type 2 diabetes mellitus: a randomized crossover study. Diabetol Metab Syndr. 2017;9:64. Published 2017 Aug 31. doi:10.1186/s13098-017-0263-8
[14] Erickson ML, Little JP, Gay JL, McCully KK, Jenkins NT. Postmeal exercise blunts postprandial glucose excursions in people on metformin monotherapy. J Appl Physiol (1985). 2017 Aug 1;123(2):444-450. doi: 10.1152/japplphysiol.00213.2017. Epub 2017 May 18. PMID: 28522762.